Note: This case study focuses on the period from the start of the COVID-19 pandemic in January 2020 through January 2021. For information on Germany’s current status, please see the country’s daily status reports and Our World In Data’s country profile.
Introduction
Throughout the COVID-19 pandemic, Germany has demonstrated elements of success across the four phases of our preparedness and response framework: prevent, detect, contain, and treat. However, starting in October 2020, the country experienced a major surge in cases and deaths that has yet to be brought under control as of January 2021.
The country’s strong enabling environment, including a good public health care system and expert scientific institutions, contributed to the early success. Germany’s prevention protocols facilitated the country’s rapid response to the outbreak, with the early development of testing capacity and high levels of testing, an effective containment strategy among older people, and efficient use of ample hospital capacity. With the surge, however, the disease began to spread among older people, and hospital capacity has been stretched.
Prevent: Local health authorities, the Robert Koch Institute (RKI)—Germany’s public health institute—and other scientific institutions produce data and analysis to inform Germany’s response. RKI and scientists at other institutions mobilized in early January 2020 to launch a national crisis management effort to understand the epidemiology of the pandemic.
Detect: One of the first diagnostic tests for COVID-19 was developed at Berlin’s Charité hospital, and the government worked to mobilize the country’s public and private laboratories to rapidly scale up testing capacity. Later, Germany became a pioneer in polymerase chain reaction (PCR) testing, which continues to feature prominently in the national strategy.
Contain: For a time, Germany maintained relatively limited transmission in long-term care facilities, which kept deaths down, because older people are more likely than younger people to die from the virus. The relatively low rate of infection among Germany’s population over age 70 was probably one driver of its relatively low case fatality rate in the first surge. In the second surge, however, the country was not able to replicate this success.
Treat: With a large number of hospital beds and careful planning, Germany’s intensive care units (ICUs) were not overly stressed in the first surge, although health care workers had to contend with shortages of personal protective equipment (PPE). In the second surge, it has become clear that ICU capacity is lower than initial estimates, because there is a shortage of trained staff to care for the patients in all available beds.
Context
Germany has the fourth largest economy in the world and spends approximately 11 percent of its gross domestic product on health care, with US$5,119 spent per capita per year.2 As a result, the capacity of Germany’s health care system is considered to be very high. In the European Union (EU), Germany has the most hospital beds per 1,000 people (8.3)3 and a robust sector of private and public laboratories, among which nearly 200 have the capacity to test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19.4 As of 2017, it also ranked among the top five countries in the EU for the number of nurses (13.2) and physicians (4.2) per 1,000 people.5
Germany has traditionally held the most restriction-free and consumer-oriented health care system in Europe. Health insurance is mandatory for all citizens and permanent residents of Germany, with approximately 90 percent of the population covered through nonprofit nongovernmental insurance funds and around 10 percent of the population covered through private insurance.6 In a Commonwealth Fund survey, Germany has the shortest wait times for both consultations with specialists and elective surgeries.7
The user-friendliness of the health care system and its ample human resources and physical infrastructure have led to exceptional and continuously improving health indicators. For example, life expectancy at birth grew from 75 years in 1990 to 81 years in 2018,8 and the maternal mortality ratio also decreased from 11 deaths per 100,000 live births in 1990 to 7 in 2017.9
The first case in Germany was reported on January 27, 2020, in Bavaria. By then, Germany’s public health infrastructure had already mobilized against the disease.10 Risk assessments and technical guidelines for testing, case finding, contact tracing, hygiene, and disease management, as well as various other documents, were made available on January 16. RKI began issuing daily situation reports for the national and international public health sector on January 23.11
On February 27, with a total of 26 confirmed cases, the government set up an inter-ministerial national crisis management group. The next day, the government required all travelers entering the country from high-risk areas (such as, at that time, parts of China or Italy) to provide information about possible exposure and contact details.12 At the end of February and beginning of March, mass gatherings and travel were increasingly restricted. On March 10, mass gatherings with more than 1,000 participants were prohibited. In mid-March the federal states started to close schools. On March 18, non-EU citizens were barred from entering the EU for 30 days.13
On March 22, Chancellor Angela Merkel announced that the federal states and national government had jointly decided to implement a “contact ban,” limiting public gatherings to two people (outside families), requiring physical distance of at least approximately 5 feet (1.5 meters), and closing many businesses.14 On April 10, all travelers arriving in Germany, regardless of their origin, were required to quarantine for 14 days.
These measures paid off. By April 15, when new cases reported per day numbered approximately 2,000 (compared with a peak in March of 6,000), the government announced a gradual easing of physical distancing measures.
Germany experienced two small outbreaks during the summer. In late June 2020, outbreaks linked to slaughterhouses and low-income housing peaked at 615 daily cases (7-day average).15 In response, the government ordered the first lockdowns since the country reopened in March, tested all 7,000-plus workers at a slaughterhouse in Gütersloh, and set up new testing sites in hot spots to catch additional spread.16
In late August through early September, another small outbreak was linked to vacationers returning home from travels.17 Indeed, as travel restrictions were lifted over the summer months, the share of cases with exposure outside of Germany rose, peaking at 49 percent of cases nine weeks after they were lifted.
Beginning in early October, Germany, like much of Europe, started seeing a sustained second surge, with cases almost entirely of domestic origin (only 0.6 percent of cases were linked to foreign exposure). RKI reported that cases originated from a number of sources, including households, nursing homes, and religious events.18 As of January 11, 2021, the number of daily confirmed cases (7-day average) was 18,576, with a cumulative total of 1,941,116 cases and 41,799 deaths.19
COVID-19 Timeline
New cases per day (7 day rolling average)
Prevent
The German government entered the pandemic with a detailed National Pandemic Plan.20 Together with generic preparedness plans and other disease-specific plans and documents (e.g., for Middle East respiratory syndrome), this detailed response plan enabled the government to activate quickly, with no time wasted on disputes related to governance, accounting, or costs.21
Because Germany is a highly federalized country, the responsibility for public health lies with intermediate and local public health authorities in 16 federal states and approximately 400 counties. They adapt the national guidelines and recommendations to local needs. National authorities facilitate a nationwide exchange and negotiate standards and common procedures.
As Germany’s national public health institute, RKI is dedicated to the prevention, control, and investigation of infectious diseases. In addition to routine surveillance, its team of scientists conducts research on infectious disease pathogenesis, risk assessment, epidemiology, and sentinel surveillance systems to support the federal government, local and intermediate public health authorities, and health professionals during outbreaks.22 RKI publishes risk assessments, strategy documents, response plans, daily surveillance reports on COVID-19, and technical guidelines, communicating this information via national and international public health authorities. This steady flow of information has helped the government—as well as local and intermediate public health authorities, health professionals, and the public—make critical decisions during the outbreak.
Detect
In January 2020, scientists at Germany’s Charité hospital developed one of the first specific tests to detect the presence of SARS-CoV-2 in patients, which is now used widely around the world.23 The World Health Organization adopted it as one of the core diagnostic tests. Given how quickly the test was developed, Germany was able to turn its attention early to increasing testing capacity.19 The country was uniquely positioned to do this because its laboratories have the expertise, accreditation, and equipment to conduct PCR assays and quickly deliver diagnoses. On February 28, the government facilitated this process by mandating that all insurance companies pay for COVID-19 tests for symptomatic people,24 which in turn incentivized private laboratories to scale up quickly. The policy was later updated to include asymptomatic people and to prioritize the use of rapid tests for those in contact with high-risk people (e.g., a hospital or nursing home).25 Due to this rapid scale-up of testing capacity, Germany was able to bring its positivity rate below 3 percent approximately 50 days after daily cases surpassed 30.
When the winter surge began, Germany had a testing capacity of approximately 1.1 million tests per week, with about 90 percent of capacity coming from decentralized private laboratories.26 Despite such high capacity, positivity rates rose (see graph below) as cases increased. During December 2020 and January 2021, Germany did not meet the World Health Organization benchmark of 10 percent test positivity, and at the end of January had just dropped below the 10 percent threshold.27
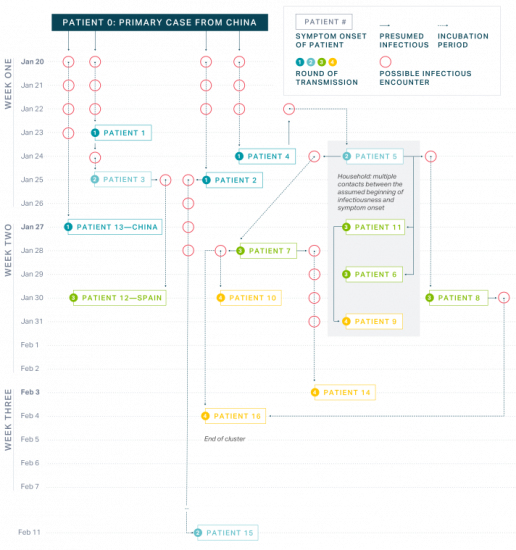
Bavarian health authorities and scientists closely examined—and eventually broke—the chain of transmission among the first cluster of cases, which occurred at the end of January 2020 in Bavaria. Breaking this initial chain bought Germany critical time to design its response while yielding important lessons about how the disease is transmitted.28 By using a combination of epidemiological methods such as interviews and whole genome sequencing, the team was able to reconstruct and describe transmission events precisely. This research provided details on attack rates, incubation periods, and the serial interval, which enabled public health experts to estimate the potential size of the epidemic and decide on appropriate containment measures.29
Even when the number of cases grew exponentially in Germany, local, intermediate, and national authorities continued to make tremendous efforts to conduct contact tracing for every single case, despite a lack of staff. Citizen science projects were launched to complement the government’s efforts. For example, RKI released the Corona Data Donation smartwatch app on April 7. The voluntary app works by collecting activity and heart rate data, along with postal codes, and analyzing the information for potential COVID-19 symptoms.31 On June 16, 2020, RKI launched the Corona-Warn-App, also for voluntary use. It works by asking individuals to report their positive test status via the app; Bluetooth connections between phones trigger alerts to people who have come into contact with someone who tested positive.32 The app also categorizes the level of exposure (by distance and time) and suggests a course of action.33 To protect data privacy, the identifiers are anonymous to users and data are deleted after two weeks.34 After 100 days, over 18 million active users had reported over 1.2 million test results.35 However, the app has faced criticism for adding to the confusing universe of apps used during the pandemic while being only minimally effective.36
The biggest need related to contact tracing is human resources at local public health facilities, many of which are understaffed. The German Federal Ministry of Health and RKI hired and trained “containment scouts”— typically medical students—to support local authorities in tracing contacts.37 Health leaders emphasized the fundamental importance of contact tracing and the need to maintain staff levels to keep caseloads low, so that contract tracers could keep up with the volume. Following up with all contacts becomes more difficult during larger outbreaks, regardless of the level of contact. As spread increased throughout November, contact tracing became all but impossible. As of November 6, 2020, an estimated 75 percent of cases were not traceable.38
German scientists from the University of Bonn conducted some of the world’s first COVID-19 antibody studies in the hard-hit town of Gangelt, where they found community infection rates of nearly 14 percent.39 In April, as part of its long-term strategy, RKI announced a three-pronged approach to gathering data about community spread, with the idea that the data will help shape more sensitive policies in the future.40 The elements of its approach were:
- Serological examination of blood donors: Starting in April 2020, approximately 5,000 blood samples from adults were examined every 14 days to learn what percentage had antibodies present. Interim results of nearly 50,000 samples, released in November 2020, showed that overall prevalence of SARS-CoV-2 antibodies was 1.35 percent, with rates higher among men and younger age groups (18 to 29 years). The study was extended through April 2021 to track how prevalence changes due to the winter surge.41
- Serological examination of COVID-19 hot spots in Germany: A representative sample of approximately 8,000 volunteers who are age 18 or older and live in harder-hit areas within Germany have been examined several times since May 2020. Interim results focused on particular regions have been released periodically, but the study is still ongoing.42
- Population representative screening: At least ten studies examining serological prevalence using population registry samples are being conducted throughout Germany, and additional studies focusing on target populations (e.g., pregnant women and school children) are underway.43
Contain
In Germany, efforts to enforce physical distancing measures are complicated by the country’s federal system. States can enact requirements that differ from national guidelines, and the chancellor must obtain unanimous consent to impose a nationwide law or ban.
On March 22, Germany enforced strict physical distancing guidelines, banning groups of more than two people in public and shutting down some businesses. Unlike many other EU countries, however, Germany never issued a curfew. These restrictions were lifted in May.
On October 28, with a 7-day average of 12,709 cases and after a doubling of hospitalizations over 10 days, Chancellor Merkel, along with state leaders, announced a tightening of social distancing requirements, closing high-risk businesses including bars, restaurants, sports venues, and gyms. The restrictions also lowered approved gathering sizes to fewer than ten people in two households.44 These actions were widely referred to as “lockdown light,” in contrast to the strict measures taken in March.45
In light of still-increasing case counts, additional guidelines were announced on November 16, discouraging private parties and encouraging people to keep all contacts to their households and limit visits to public areas.46 Even these stricter lockdown measures proved insufficient as cases continued rising. One month later, a strict lockdown was announced, with “only essential businesses such as supermarkets and banks” allowed to remain open.47
Each additional restriction faced protests from right-wing groups.
Travel bans were put into effect in the spring but loosened in May, along with other reopening measures. As a result, travel during the summer months was largely unrestricted. In August, Germany updated its guidelines for travelers to require a test (August 8) and 5-day minimum quarantine (announced August 24) for travelers returning from high-risk areas.48 On November 8, this was further revised to require travelers to use digital entry registration if they had been to a high-risk area in the past 10 days.49 With high case counts throughout the end of 2020, state and federal leaders agreed on a new testing strategy for travelers in January 2021, the “two-test strategy.” Travelers are required to take a test upon entry or 48 hours prior to arrival and take a second test to exit quarantine prior to the 10-day recommendation. As of early 2021, travel bans were put in place for South Africa and the United Kingdom, areas with widespread, known variants.50
Initially, Germany was able to keep deaths low by limiting the absolute number of infections of people age 70 or older, the group with the highest fatality rates. Of Germany’s total number of cases as of May 2020, 19 percent were among people 70 or older, compared with 36 percent in Spain and 39 percent in Italy. As a result, the overall case fatality rate in Germany was 4.6 percent, compared with 14.1 percent and 12 percent in Italy and Spain, respectively.51 In June, the percentage of total deaths from communal home residents (a category that includes nursing home residents, homes for people with disabilities, and others) was 39 percent.52
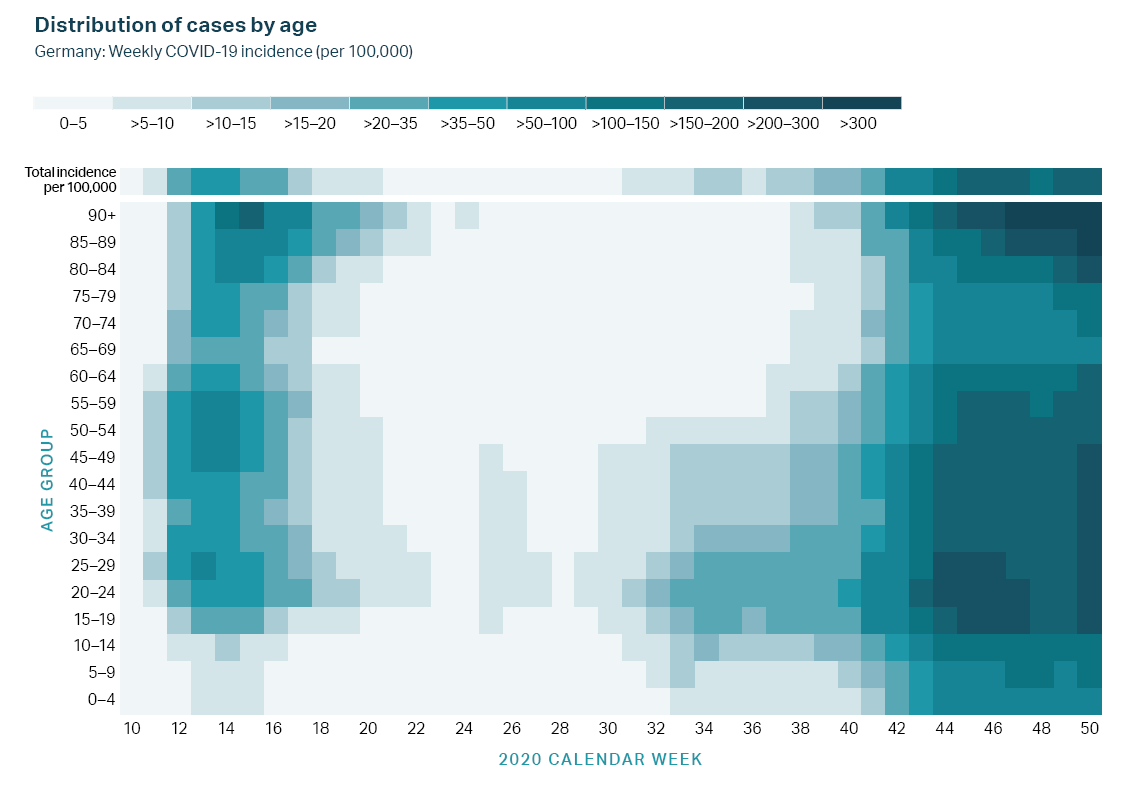
In Germany the first outbreaks affected travelers, festivals, and workplaces, not nursing homes, which may have helped limit infections among older people. Eventually, there were more outbreaks among older people, but the majority of early cases occurred in other settings.54 Germany was also able to manage infection rates in hospitals and long-term care facilities. According to RKI’s national guidelines, people who have recovered from COVID-19 and who return into care homes from hospitals must have tested negative or have undergone a 14-day quarantine.55 Furthermore, specific guidance is provided to nursing homes on hygiene measures and protocols to handle suspected and confirmed cases as well as outbreaks.56 Older people were also tested more often than younger age groups.
Illness among older populations, however, has been rising since September (along with overall case counts), with nursing homes tied to recent outbreaks.57 Only 12 percent of all cases were among people 70 years or older, but 86 percent of deaths occurred within this age group.58 Despite rising case counts, protocols for long-term care facilities have remained the same as in the early phases of the pandemic.
When vaccinations began, older people, and nursing home residents in particular, were prioritized. Vaccinations in all states began on December 27, although Germany is vaccinating at a slower rate compared with several of its peers. The first vaccine available was the Pfizer-BioNTech vaccine, which was developed in Germany; the Moderna vaccine was delivered to Germany starting on January 11, 2021.59 The country is part of the EU’s joint procurement process and is slated to received 64 million Pfizer doses and 50 million Moderna doses. To supplement this, Germany’s federal government purchased 30 million Pfizer doses outside the joint process. The joint process has been criticized for not securing enough doses of the Pfizer vaccine, and in-country distribution has faced challenges reaching the stated goal of 300,000 doses per day, in part due to supply shortages and holding back vaccine for second doses.60
Schools reopened in August 2020 after summer break and have mostly remained open. As of November 13, nearly 10 percent of schools had known cases, although very few cases were linked to transmission within schools. The specific guidelines pertaining to schools are determined at the state level, and practices vary by state. Many schools do not require masks in the classroom but do require them in common spaces like halls. Ventilation has been a priority for classrooms,61 and Germany has committed 500 million euros (€) in federal funds to improve ventilation in public buildings, including schools.62
Like nearly all business, most schools were made to close starting on December 13, 2020.63 The second wave of reopening began in early February 2021, but most states have kept schools closed in the midst of discussions to extend the strict lockdowns and evidence suggesting that the new variants may be more transmissible in children.64
Treat
In March 2020, a register of ICUs was established by the German Interdisciplinary Association for Intensive Care and Emergency Medicine and RKI.65 Since April 16, 2020, ICU capacity and COVID-19 patients treated in ICUs have been reported daily. These data help make clear the severity of the disease and potential impacts on the health care system. Based on daily reports showing a long-term trend of sufficient ICU capacity, the government passed a law on May 14, 2020, providing free ICU care to patients from other EU countries.66
The management of PPE supplies has not been as successful. The government launched a crisis team to centrally procure PPE, and on March 4, 2020, it banned the export of all PPE.67 Despite these measures, Germany has seen shortages of more than 100 million single-use masks, 50 million filter masks, and 60 million aprons and disposable gloves, leading to a protest by health care providers on April 27, 2020.68 German authorities continue to work on procuring these supplies, but like many other countries around the world, they have yet to entirely solve the problem.
As cases rose in late 2020, the strain on the health system also increased, with 75 percent of registered ICU beds occupied (from all causes, approximately 16 percent of which were COVID-19 cases). The number of COVID-19 patients in ICUs (3,385 as of November 15, 2020) surpassed the number in March 2020 during the first peak. By December, reports of hospitals turning down non-COVID patients and reaching full capacity based on staff availability were shared by the German Hospital Federation. In some states, hospitalized COVID cases were five times the springtime levels.69
Health System and Economic Impact
After doctors saw a decline in specialist visits throughout the spring, doctors publicly encouraged people in late May 2020 to visit a doctor as needed, because hospitals had plenty of capacity at that point and the risk of infection was low.70 By October, Germany was accepting patients from other countries, given its excess ICU capacity.71
During the winter surge, however, the health system began to feel strained. Hospitals pulled back on regularly provided services to accommodate COVID-19 patients. It also became clear that the number of ICU beds available was not an appropriate measure of the capacity of the health system, because some facilities with beds are short-staffed and cannot adequately treat the number of patients for whom there are beds.72 In March 2020, the economic rescue package included €9.5 billion toward the health system, including €3 billion toward hospital investments.73
Economically, Germany is expected to perform better than many of its European peers, in large part due to government safety nets and stimulus packages that provided business and job protection, direct relief payments, and tax cuts to keep consumer spending at reasonable levels. The government has passed two economic packages—an approximately €800 billion rescue package in March 2020 and a €130 billion stimulus package in June 2020. Germany is estimated to have provided the equivalent of 30 percent of its 2019 GDP in fiscal support.74
Although the economy has performed relatively well, unemployment is high and still rising, and the full impact of the 2020–2021 winter surge remains to be seen.
Conclusion
Germany demonstrates the difficulty of maintaining success throughout the COVID-19 pandemic. Despite early success relative to its peers in the first phases of the pandemic, the country experienced a major spike in cases that began in October 2020, and as of early February 2021, average daily case counts remained above the April 2020 peak. Overall, although Germany cannot be considered a positive outlier, it has still done well relative to most of the hard-hit countries in the EU.75
Early on, Germany’s strong health care system and early progress on detection complemented its effective containment strategy. Ensuring the increase of human resources among understaffed local public health facilities was another key component to enable more efficient contact tracing, but these resources were noted as potentially unstable, and indeed the health system was stretched past capacity in several areas during the winter surges.
In general, Germany’s focus on collecting and analyzing data and communicating the results to the public has led to high levels of trust in the government throughout most of the pandemic. In May 2020, Germany moved forward with relaxing its physical distancing guidelines based on data collected on case counts and growth. Chancellor Angela Merkel regularly cites RKI surveillance data and uses epidemiological concepts such as reproduction rate as a driving factor behind decisions related to social distancing measures.76 The German government has focused on three indicators—infection rate, disease severity, and health system capacity—to measure the quality of its response. Setting clear expectations and providing transparency to the public on the criteria for government decision making about reopening is a key factor in gaining public trust. There were, however, challenges reinstating restrictive measures once the second surge occurred, with more prominent political resistance and states deviating from federal recommendations.
Germany’s federal system has led to varied approaches and guidance from each state related to social distancing. While this allows for tailored strategies, it has also limited widespread implementation of a standard testing strategy or nationwide containment measures even in the face of rising case counts.
Further, Germany’s low case counts in the spring of 2020 meant that most of its population remained vulnerable to infection, which enabled the rapid spread seen in the fall and winter of 2020. Potential explanations for the surge include the switch from outdoor to indoor activities as the weather got colder, higher levels of travel coming back from summer holidays, and a lag in the reinstatement of strict containment measures until after case counts outran contact-tracing capabilities.77
In-depth explainers on Exemplar countries
This framework identified three countries which provide key success stories in addressing the pandemic: South Korea, Vietnam and Germany. In follow-up articles, in-country experts provide key insights into how these countries achieved this.