Note: This case study focuses on the period of time from the start of the COVID-19 pandemic in January through mid-December 2020. For information on South Korea’s current status, please see the country’s daily status reports and Our World In Data’s country profile.
Introduction
South Korea’s response to COVID-19 has been impressive. Building on its experience handling Middle East respiratory syndrome (MERS), South Korea was able to flatten the epidemic curve quickly without closing businesses, issuing stay-at-home orders, or implementing many of the stricter measures adopted by other high-income countries until late 2020. It achieved this success by developing clear guidelines for the public, conducting comprehensive testing and contact tracing, and supporting people in quarantine to make compliance easier. The country successfully managed outbreaks in March and August and gradually gained control of a larger, more dispersed outbreak in December 2020. Overall, South Korea has shown success across three phases of the epidemic preparedness and response framework: detection, containment, and treatment.
- Detect: South Korea built innovative, high-capacity screening facilities and worked closely with the private sector to ensure an adequate supply of tests from the onset of the pandemic. The country maintains approximately 600 screening and testing centers and 150 diagnostic laboratories, with capacity reaching 110,000 tests as of November 2020.
- Contain: South Korea isolated infected patients, increased compliance by supporting those in quarantine, and traced contacts with unusual thoroughness. Hundreds of epidemiological intelligence officers were deployed for these tracing efforts and empowered to use a wide variety of data sources, including credit card transactions and closed-circuit television footage.
- Treat: The health system surged to meet demand, especially in Daegu, the site of a large cluster of infections in March 2020. An additional 2,400 health workers were recruited in Daegu alone. Across the country, the government restructured the hospital system, built temporary hospitals to increase capacity, and addressed shortages of personal protective equipment (PPE) through centralized government purchasing.
South Korea’s strong enabling environment positioned the government to act quickly and effectively. After its flawed response to a MERS outbreak in 2015, the government made 48 reforms to boost public health emergency preparedness and response. In addition, a well-functioning national health insurance system, ample human resources and infrastructure, and constructive relationships between key institutions—such as the president’s office, the Ministries of Health, Education, and Foreign Affairs, and the Korean Centers for Disease Control and Prevention, which was renamed the Korea Disease Control and Prevention Agency (KDCA), during the pandemic—enabled an extraordinarily decisive response to the pandemic.
Context
Since the 1960s, South Korea’s economy has grown at a remarkable pace, and it is currently the 12th largest in the world.2 Health outcomes have improved alongside economic progress. South Korea put social health insurance in place in the 1970s, achieved universal health care coverage in 1989, and transitioned to a single-payer system in 2004.3
South Korea’s health system is centered on hospital-based care. The number of hospital beds per capita, 12.3 beds per 1,000 population, is two times higher than the average in Organisation of Economic Cooperation and Development (OECD) countries.4 The country excels not only in hospital capacity but also in interactions with doctors, with an OECD-leading 16.6 consultations annually per capita.5 Although some critics suggest that South Korea’s health system is overly dependent on secondary or tertiary facilities instead of primary facilities, this extra capacity enabled hospitals to respond quickly to COVID-19 without sacrificing care for non-COVID-19 patients.6
Despite its robust health system, South Korea struggled to respond appropriately to the 2015 outbreak of MERS, which resulted in nearly 17,000 suspected cases and 38 deaths. During the six months of that outbreak, Koreans lived in fear, and the government lost an estimated US$2.6 billion in tourism revenue while spending almost US$1 billion on diagnosis, treatment, and other parts of its response.7
After MERS, the country made a total of 48 reforms to improve pandemic preparedness and response, including more infection control staff and isolation units, expanded outbreak simulations and PPE training, and community-based collaboration between medical centers and local governments.8 When COVID-19 struck, the painful memory of MERS inspired an early and aggressive government response—and a willingness among people to wear masks, cooperate with contract tracers, and otherwise listen to public health officials. For example, wearing a mask in public spaces, already common because of air pollution, became a social norm early in the pandemic.9 A poll showed that more people adhered to public prevention protocols during the COVID-19 outbreak than during the MERS outbreak.10
South Korea was one of the first countries to experience a COVID-19 outbreak, with its first case, imported from Wuhan, China, reported on January 20, 2020 (see Figure 1). The government activated the Central Disaster and Safety Countermeasures Headquarters within days, and it has met daily since then, with the prime minister attending at least three times a week.11
The number of confirmed cases ranged from zero to two per day for the first month of the outbreak, until a cluster was identified in Daegu, a city of about 2.5 million, starting at 15 cases on February 19. The cluster originated from the individual known as patient 31, who traveled around the cities of Daegu (including the Shincheonji Church of Jesus) and Seoul before her diagnosis.12 Thereafter, daily confirmed cases rose rapidly and reached a peak of 909 on February 29.
After this peak, the number of new cases fell rapidly in the following two weeks until it hovered below 200 daily confirmed cases by March 12. Daily cases continued to decline steadily to nearly zero, although there was a minor resurgence in mid-May (about 30 cases per day) as the country started to reopen.13
COVID-19 Timeline
New cases per day (7 day rolling average)
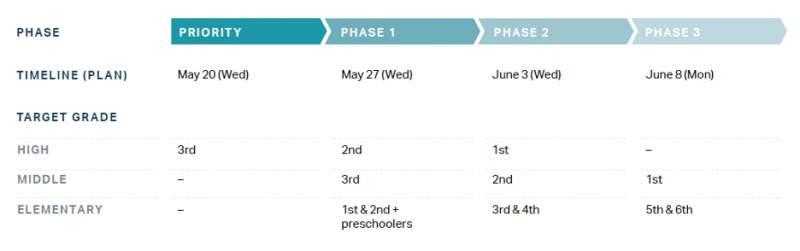
On May 6, the national mandates on social distancing were relaxed in favor of softer guidelines. Schools began holding in-person classes on May 20, which was relatively early. By June, only 20 countries had reopened schools—and 4 had never closed them down.14 The return to in-person classes in South Korea was staggered by grade and completed by June 8, 2020,15 with density restrictions (e.g., staggering days on which students attended in person) in areas of higher community transmission.16 Studies conducted over the summer found that reopening schools had a limited impact on the development of new disease clusters.17 In the semester starting September 2020, schools were given more autonomy over opening procedures and lighter capacity restraints, with guidelines set by the Ministry of Education based on the level of social distancing in effect.18 Throughout the closure and reopening process, government support for childcare, internet, and technology was provided to families in need.
In mid-August, another spike in cases led to a peak average case count of 343.9 on August 28.20 Like the Daegu outbreak, this outbreak was also linked to a religious group, the Sarang Jeil Church in Seoul. In response, Seoul reinstated its Level 2 restrictions (out of three levels), which includes limiting indoor gatherings to 50 people and outdoor gatherings to 100. It also collected the names of approximately 4,000 church members and tested about half of those, although contact tracing efforts were resisted by the church.21 Level 2 restrictions were reinstated on August 23, and by September 20, daily cases had fallen below 100.
In September 2020, the Korean CDC, previously under the Ministry of Health and Welfare, transitioned to a stand-alone agency called the Korea Disease Control and Prevention Agency (KDCA), with increased staffing. KDCA releases daily reports that not only outline the raw numbers (e.g., cases, deaths, patients by severity), but also identify the location and case counts by different clusters and remaining health system capacity such as bed counts in intense care units.22
Daily cases hovered around 100 in mid-November, when South Korea began to experience its third significant outbreak, with daily case counts that peaked at over 1,000 before decreasing in January 2021.23
Detect
KDCA received viral specimens from China to begin developing diagnostic tools even before the first case was confirmed in South Korea. As soon as the first case was reported, South Korea turned its focus toward preparing for large-scale testing. Many biotechnology companies sprang up in the years between MERS and COVID-19,24 enabling the development of public-private partnerships and scaled-up testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19.
On January 27, 2020, a week after the first COVID-19 case in South Korea, KDCA directed private companies to produce a diagnostic reagent.25 Within two weeks of the first case, thousands of test kits were shipped daily, with the number reaching up to 100,000 kits per day in March.26 By April 24, 118 institutions were able to run an average of 15,000 tests (and up to 20,000) per day. The number of institutions running tests continued to climb gradually, reaching 146 by August.27 Subsequently, testing capacity increased 600 percent, reaching 110,000 per day by November 2020.
After testing capacity was expanded, the focus shifted to screening. To prevent infected people from entering hospitals, for example, COVID-19 screening clinics were set up outside entrances. Those flagged based on their symptoms or responses to screening questions were tested and told to return home and self-quarantine while they waited for results, whereas those who were considered low risk received a day entrance pass. Screening stations were set up in various strategic locations, including at Incheon International Airport. By September 22, there were 599 screening stations, including 48 drive-through centers. To encourage full testing among migrant worker communities, where several clusters emerged, the government announced that it no longer required health workers to report known undocumented residents.28
During the surge of cases in Daegu in February 2020, health officials opened 600 screening centers using innovative approaches to increase capacity.29 For example, drive-through testing centers collected three times as many samples as conventional ones, while removing the need for negative pressure rooms that prevented contaminated air from escaping into uncontaminated areas.30 Meanwhile, phone booth–style stations enabled health care workers to evaluate and test people without coming into direct contact with them. First, workers stood outside negative pressure booths wearing PPE. Eventually, they shifted to positive pressure booths, which minimized the need for PPE and thereby prevented fatigue.31 By late March, the country had performed over 300,000 tests, equal to a rate more than 40 times higher per capita than in the United States at that time.
Since March 15, the test positivity rate has been below 2 percent, and from April 6 to August 15, it was 1 percent or lower. During the second spike in August, the positivity rate peaked at 2.5 percent, and it reached 3.3 percent during the December surge, both well below the World Health Organization benchmark of 10 percent test positivity for adequate testing levels.32
Contain
In late January 2020, South Korea instituted special entry procedures for travelers coming from Wuhan. Procedures initially included designated entry lines and questionnaires and later expanded to include temperature checks, testing all travelers at the border, and mandatory quarantines monitored for 14 days. (Travelers without Korean residency are provided facilities for self-quarantine but must pay for the cost of their stay.) This policy of tracing and quarantining, rather than restricting entry, is in line with recommendations from the WHO, whereas border closures are not.33
As case counts increased globally in the summer and fall of 2020, South Korea tightened travel restrictions and as of October 2020, requires visas for nearly all foreign nationals. It suspended visa-waiver countries and visa-free countries, with some exceptions (e.g., flight attendants). Visa applicants are required to submit forms about their health status and show symptom-free certification from a medical professional. Overall, visitors to South Korea decreased by 81 percent year-over-year.34
In the early months of the pandemic, the South Korean government transformed public facilities and retreat centers owned by private corporations into temporary isolation wards. It did this for two reasons: to care for COVID-19 patients while preventing transmission within households, and to relieve hospitals of bed shortages. Health care workers regularly monitored and quarantined clinically stable patients who did not require inpatient treatment.35
In Daegu, the site of the first cluster, 15 community treatment centers, including several in dormitories for training institutes of private companies such as Samsung and LG, admitted 3,033 people between March 3 and March 26, 2020. Health professionals monitored the centers and patients reported their symptoms regularly by a smartphone application or by phone. The facilities were equipped with pulse oximeters, X-ray machines, and RT-PCR tests for SARS-CoV-2. Only 81 of 3,033 (2.67 percent) cases were transferred to a hospital for higher-level care.36
South Korea’s quarantine policies are strict but supportive. People who have been in contact with a confirmed case, traveled internationally, or suspect they might be infected are required to self-quarantine. Those in quarantine are required to use the Self-Quarantine Safety Protection app for 14 days. Case officers monitor the app, including location tracking, to identify when people break quarantine. Violators are required to wear “safety bands,” electronic wristbands that connect to the app and alert case officers if they are not in the same location as their mobile devices. The fine for violating self-quarantine is heavy: US$8,217.37
At the same time, case officers provide support to make quarantine easier. Twice daily they check in with those who are self-quarantining, to deliver food and toiletries and offer psychological counseling and video-streaming services for entertainment.38
South Korea has maintained a focus on mental health throughout the pandemic, creating hotlines and recordings for those in isolation as early as January and maintaining a national psychological support team.39
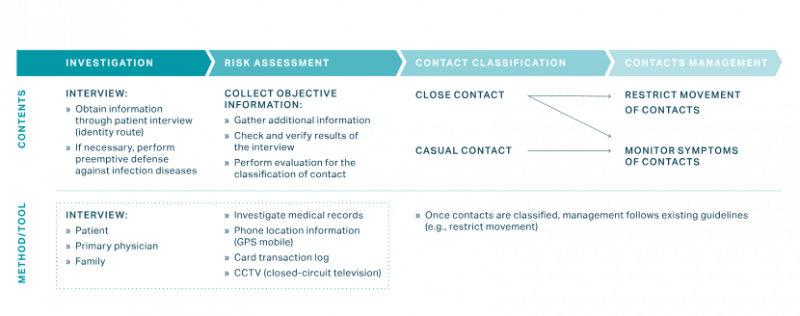
South Korea took an aggressive approach to contact tracing early in the outbreak. First, they scaled up their network of contact tracers. Second, they gave these workers access to data beyond what they might be able to learn from a typical patient interview. Third, they used public communications to empower citizens to assist the health system with contact tracing.
South Korea expanded its usual workforce of Epidemic Intelligence Service (EIS) officers by quickly training staff at approximately 250 local public health centers, hiring 300 private epidemiologists, and leveraging staff at 11 nongovernmental organizations that train and support EIS officers. This multilevel approach was effective, with the veteran EIS officers conducting the more difficult investigations in large clusters, and health facilities and temporary staff handling smaller clusters including families. These efforts led to earlier case detection, kept the rate of new infections low, and potentially reduced estimated mortality rates by preventing hospital overcrowding and infections among high-risk populations.41
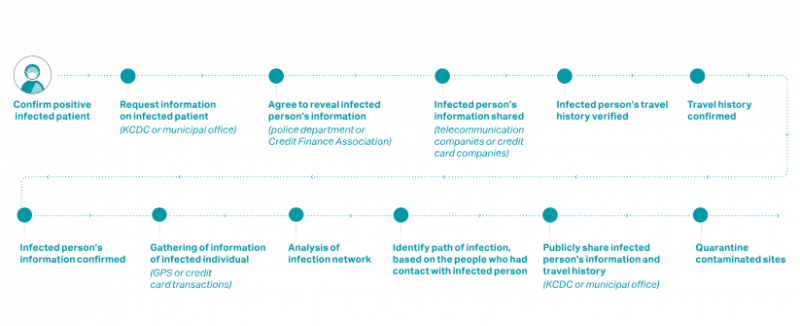
The work of the EIS officers was further facilitated by legal changes following the 2015 MERS outbreak. When necessary, the officers were permitted to draw on four major types of information in addition to patient and doctor interviews:
- Facility visit records, including pharmacies and medical facilities
- Cellular GPS data from cell phones
- Credit card transaction logs
- Closed-circuit television
This information was combined with interviews and cross-checked with other data to trace contacts and take appropriate containment measures.43 (see figure below)
On June 10, 2020, the country introduced an additional system called KI-Pass to help contact tracing efforts after outbreaks at several high-risk locations. The system introduces QR codes at high-traffic facilities like bars and gyms to replace manual sign-in sheets.45 To respond to public worry about data use and privacy, the government instituted additional data protections, including automatically deleting data after 14 days.46

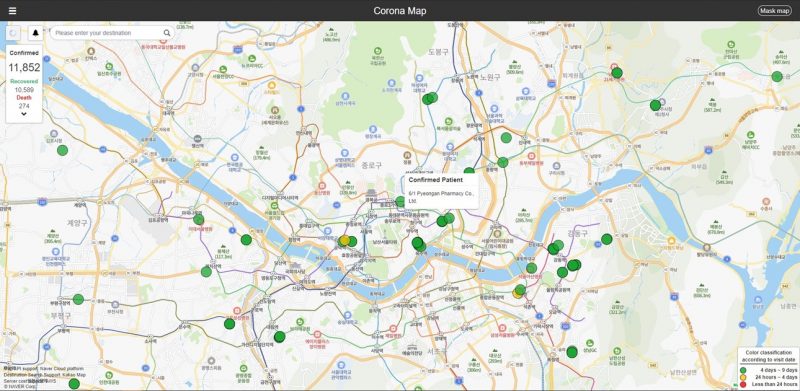
South Korea encourages compliance with containment efforts by developing apps that collected relevant data, which eases the burden on EIS officers and made it possible for them to cope with the high volume of investigations. Patient trajectories are made public to enable citizens to track their own movements compared with those of suspected cases. Traveler information is shared with health facilities and pharmacies to facilitate prompt identification of cases and contacts.48
Korea has a three-tiered social distancing system with half levels (i.e., Level 1, Level 1.5, and so on through Level 3), as well as a “distancing in daily life” strategy, designed to be the most sustainable level of restriction. These levels are adjusted based on metrics including the number of cases and rate of change.49
In May and June, after the first implementation of the “distancing in daily life” strategy, multiple outbreaks occurred in the Seoul area, with clusters from bars and warehouses. As a result, Seoul resumed more strict distancing guidelines until daily case counts were below ten. During the second spike in August, the entire country moved up to Level 2. These restrictions were eased in most of the country on October 1250 but tightened again to Level 2 in November and Level 2.5 in Seoul in December as infections among asymptomatic young people increased.
Throughout the pandemic, information on proper mask-wearing and distancing was widely shared, and the government worked to find sources of misinformation. When misinformation was identified, the Korea Communications Standards Commission addressed the issue with cooperation from major websites like Google and Facebook.51 In October, Korea amended its Infectious Disease Control and Prevention Act to introduce mandatory mask-wearing, enforceable by fines of up to 100,000 Korean won (KRW), approximately US$90.52

Treat
During a shortage of hospital beds in the epicenter of Daegu, health officials developed a triage system using a brief severity scoring system to classify patient illnesses as mild, moderate, severe, or critical. Mildly ill patients were sent to community treatment centers where they were closely monitored, moderately ill patients were sent to community hospitals, and severely or critically ill patients were hospitalized at tertiary hospitals equipped to provide intensive care.54
Using portable negative pressure devices, the government was able to rapidly expand the supply of temporary airborne infection isolation rooms. In Daegu, officials created about 400 additional negative pressure beds during the crisis.55
Daegu officials also recruited about 2,400 additional health care workers who were spread out among screening clinics, infectious disease hospitals, and community treatment centers. In addition, 327 physicians volunteered without pay to participate in the public health response, with 30 volunteering for the centralized COVID-19 response team and 260 volunteering for phone triage centers.56
As with many cities around the world during the COVID-19 pandemic, Daegu faced a shortage of PPE, a critical issue that was escalated to the national government. Initially, the government limited the export of masks and penalized hoarding among retailers, but in mid-February, emergency measures doubled the production of masks in South Korea to an average of 10 million per day by March.57
The government intervened in early March to purchase 80 percent of the mask supply from Korean manufacturers, fully ban exports, set a price limit on mask sales, and limit the number of masks sold weekly through retailers. Moreover, the government prioritized the distribution of masks to medical facilities. These interventions provided relief and averted further shortages, without forcing hospitals to issue policies about reusing PPE.58 As the mask supply stabilized, the government relaxed sales limits to three masks in April and ten in June, and eliminated specific purchasing days. This policy was enforced by the development of a shared database that logged purchases across markets, post offices, and pharmacies.59
After the Daegu surge, South Korea took a series of steps to manage capacity in the health system. The Central Disaster and Safety Countermeasure committee restructured the health care system to form six regional clusters (instead of 17 state and city jurisdictions) to make it easier to transfer patients between facilities and manage capacity.60 Currently, a variation of the severity scoring system first used in Daegu is in use nationwide, with four different categories: asymptomatic, mild, moderate, or severe. Asymptomatic and mild cases are placed in one of five residential treatment centers instead of hospitals.
As of September 22, 2020, in addition to the 198 beds that compose the National Designated Isolation Unit, 43 hospitals with 4,075 hospital beds were designated Infectious Disease Hospitals and dedicated to COVID-19 treatment.Similarly, 323 hospitals were designated National Safe Hospitals for people seeking non-COVID-19 treatment. Each of these hospitals has separate areas for those with respiratory symptoms to be evaluated.61
Health and Economic Impact
So far, disruptions of the health system have been limited. Given the relatively low incidence of COVID-19 and rapid control of major outbreaks through the fall season, hospitals were not overwhelmed. In addition, South Korea’s policy of designating COVID-19 and non-COVID-19 hospitals helped maintain the normal functioning of the health system for all needs.
Economically, South Korea is expected to be one of the better-performing countries in 2020. In August, the OECD projected that it would face the least economic impact, as measured by the percentage decrease in GDP for all 37 OECD member countries.62 In October 2020, South Korea reported a growth of 1.9 percent from the previous quarter. Much of this growth has been driven by exports of memory chips for electronics and of automobiles to Europe and the United States.2
Part of the explanation for this success is that South Korea was able to avoid some of the severe long-term restrictions, such as lockdowns and business closures, that have led to troubled economies in many high-income countries. For example, after the government tightened restrictions in August because of the church outbreak and in late September because of a national holiday, it loosened them again in October.63 In fact, the country never activated its highest level of restriction—which would have barred gatherings with more than ten people and closed gyms and other high-traffic businesses.64
South Korea faced significant economic disruption, however, including large job losses. The government responded by providing subsidies to businesses for payroll and to unemployment insurance and low-interest loans to low-income job seekers. The government also lowered insurance premiums for social safety net programs for individuals and businesses. All households, regardless of income, received a disaster relief payment of KRW 400,000 (US$344) for single-person households, KRW 600,000 (US$516) for two-person households, KRW 800,000 (US$688) for three-person households, and KRW 1 million (US$859) for households with four or more members.
Conclusion
South Korea clearly stands out in the global COVID-19 response, with fewer than 80,000 cases and 1,500 deaths a full year after the first case was reported. The keys to the response have been clear, effective communication with the public about prevention best practices, aggressive and creative testing and contact tracing, and a strict quarantine policy accompanied by ample support that made it easier for patients to comply with the policy. This suite of tools has kept the disease burden low and enabled the government to manage a series of outbreaks while not unnecessarily harming the economy, which is performing better than that of most peer countries.
Despite its success, lessons from South Korea may not be relevant to all countries. South Korea, which is separated from China by North Korea, is effectively an island with respect to border travel and access. The population is highly urbanized, with over 80 percent living in urban areas.65 As a result, most cases in South Korea were clustered and often related to a small number of high-transmission events or locations, including megachurch services, other religious observances, a hobby sports group meeting, and workers in the tightly packed telecommunication center of a bank. Meticulous contact tracing may have been easier than in other settings where the disease spread through multiple smaller clusters and community transmission—as evidenced by the challenges South Korea faced in December when community spread occurred in small clusters.
Culturally and legally, South Korea is more tolerant of personal data-sharing, and its success has been heavily dependent on its ability to rapidly scale up technological solutions. Countries with less technology and where citizens do not have smartphones or are not as willing to share their data may experience difficulties adapting such strategies.
Despite these differences, many aspects of South Korea’s response are worthy of study, including its investments in preparedness, decisive and data-driven leadership, strategic clarity (a focus on testing and contact tracing), and willingness to be innovative. The data-driven agility that has led to South Korea’s success so far is being tested as cases continue to surge globally. Although the country’s case numbers are still much lower than those in many comparable countries, changes in the disease’s epidemiology—with asymptomatic young people seeding small clusters—require more innovation.
In-depth explainers on Exemplar countries
This framework identified three countries which provide key success stories in addressing the pandemic: South Korea, Vietnam and Germany. In these related articles, in-country experts provide key insights into how these countries achieved this.