Smallpox is the only human disease that has been successfully eradicated.1
Smallpox, an infectious disease caused by the variola virus, was a major cause of mortality in the past, with historic records of outbreaks across the world. Its historic death tolls were so large that it is often likened to the Black Plague.
The eradication of smallpox is therefore a major success story for global health for several reasons: it was a disease that was endemic (and caused high mortality rates) across all continents; but was also crucial to advances in the field of immunology. The smallpox vaccine was the first successful vaccine to be developed.
In this entry we cover:
- the historical and epidemiological context of smallpox disease [jump to section]
- a global overview of the long-run data on smallpox cases and mortality rates [jump to section]
- the global decline of smallpox and its eradication in 1977 [jump to section]
- the journey through varioliation to vaccination that led to its eradication [jump to section]
- the impact of smallpox vaccination on life expectancy [jump to section]
- the estimated costs of and lives saved from smallpox eradication [jump to section].
All our charts on Smallpox
What is smallpox?
Smallpox is a disease that is caused by the variola virus. It is an infectious (also known as ‘communicable’) disease meaning it can spread from one person or animal to another, either directly or indirectly. The variola virus, however, infects only humans (meaning animals are unable to catch smallpox).
There are two types of variola viruses – variola major and variola minor – with the former type being a much more severe form.
Humans are infected with the variola virus by coming in touch with droplets of a smallpox-infected patient. A healthy person can become infected if they inhale fluid droplets from another infected individual (e.g. through coughing or sneezing).2
Symptoms
Smallpox is most known for a rash of pustules covering a patient’s entire body. After being infected with the variola virus, patients usually had no symptoms for 10-14 days (an incubation period) and symptoms of a common cold for 2-3 days (unspecific symptoms).3
On average, it then took the rash 24 hours to cover the body and an additional three weeks for pustules to grow in size, form crusts and eventually fall off. A surviving patient would be marked for life with depigmented skin and scars in places where pustules had formed.
While an infection of the variola minor virus would lead to death with a probability of less than one percent, the case fatality rate of the variola major virus has been estimated to be around 30 percent.4
The specific way a smallpox infection would lead to a patient’s death remains unclear.5
The Oxford Textbook of Medicine notes symptoms of prostration (total exhaustion), toxaemia (usually poisoned by bacterial toxins) and hypotension (low blood pressure) but the exact biological mechanism causing such symptoms are unknown.6
Death usually occurred 10 to 16 days after the onset of symptoms.7
If a patient successfully fought off the infection and survived, (s)he would never catch smallpox again. A side effect of the body’s fight against the variola virus was that memory cells were produced that were able to quickly detect and activate killer cells for any variola viruses that a survivor encountered in the future.
There was never a treatment for smallpox. Once a person was infected it was impossible to treat them; one could only helplessly let the disease run its course. It might be possible that modern antiviral drugs would now allow a treatment of the disease if the disease still existed: The Centers for Disease Control and Prevention (CDC)8 now lists three antiviral drugs as potential treatment options, but since they have never been tested on infected humans, their effectiveness remains unknown.
Origins of smallpox
The origin of the variola virus and the time since when it infected humans are uncertain. The WHO9 considers two theories for its origin: either, humans were infected by a variola-like virus from rodents “16,000 or 68,000 years before present”10 or by a proto-variola mutated into the disease we now know as smallpox.
The fact that the variola virus has remained distinct from the other members of its orthopoxvirus family for 3,000 years makes the former hypothesis more likely than the latter.11
Epidemiologists hypothesized the virus’s origin by making use of the fact that it exclusively infected humans and therefore depended on a sufficiently large human population which could continuously provide new human hosts for it to survive (infected humans either die or recover and become immune for life). Egypt hosted one of the earliest concentrations of human civilization along the River Nile about 3,000 years ago, making it a likely candidate for the origin of the continued existence of various infectious diseases, including smallpox and polio.
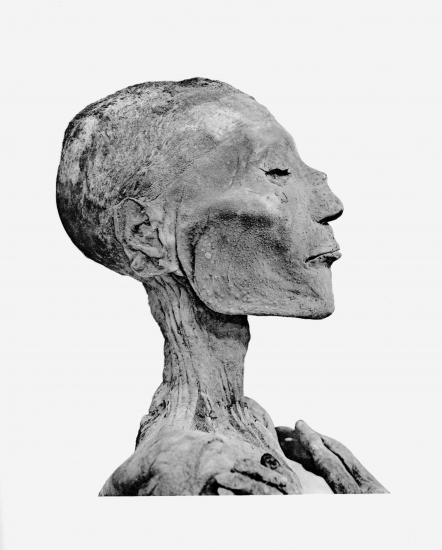
This hypothesized origin was supported by archeologists finding “dome-shaped vesicles […] similar to those found in smallpox”12on three mummies whose skin, bones and muscles were preserved thanks to the Egyptian mummification practice. One of these was Pharaoh Ramses V who died in 1157 BCE. The photograph of his skull below clearly shows small pustules, especially on his cheeks. At the time of the mummy’s discovery, electron microscopy was unfortunately not yet available. This analysis would have allowed for a definite diagnosis; authorities have not allowed investigators to extract tissue samples from the mummies since then.13
Ramses V is believed to be the first known victim of smallpox after examining the pustules found on his cheeks.14
How many died of smallpox?
In his review paper ‘The eradication of smallpox – An overview of the past, present, and future’ Donald Henderson reports that during the 20th century alone “an estimated 300 million people died of the disease.”15
In his book Anderson suggests that in the last hundred years of its existence smallpox killed “at least half a billion people.”16 500 million deaths over a century means 5 million annual deaths on average.
Long-run smallpox deaths in Europe
The graph shows the deaths per 1000 citizens from over the long-run, dating from 1774 to 1900 in European countries for which data was available. Two phenomena are illustrated here. First, Swedish data which pre-dates an effective means against smallpox (in 1796) shows the large disease burden and endemicity of smallpox in the 18th century. In peak years, up to 7 out of 1000 Swedes died of smallpox and the volatile nature of outbreaks is a symptom of a disease being endemic (explained in our section on epidemiological definitions further below).
Second, it can be seen that among selected countries, those that had adopted vaccination legislation earlier saw their smallpox death rates decrease more substantially and suffered fewer casualties during the Franco-Prussian War of 1870/71. Austria and Belgium, both of which never made smallpox vaccination mandatory, still recorded large numbers of smallpox deaths from 1875 onwards whereas other European countries displayed had already driven down smallpox fatalities significantly by then.
Nevertheless, smallpox was still endemic in every European country at the end of the 19th century.
Number of smallpox cases
The chart depicts the number of smallpox cases by country, for most countries dating 1920 until 1977. Here we see that by the time the World Health Organization (WHO) launched its Intensified Smallpox Eradication Program in 1966, most countries in Western Europe and North America had almost eliminated smallpox whilst the countries across South America, Africa and Asia, especially India, still recorded very large numbers (note the large differences in color brackets below).
Global data on the number of smallpox cases is shown in the chart. Shown here is the number of reported smallpox cases worldwide from 1920 until the last case in 1977. Just the reported number of smallpox cases between 1920 and 1978 already amounted to 11.6 million cases; and that number was certainly smaller than the actual number of cases, although we do not know by how much. Even though smallpox had a high visibility and should therefore be relatively easy to document, the lack of an international organization dedicated to global health means the number of reported cases is probably substantially lower than the true number of cases. Crosby (1993) estimates that in 1967 10-15 million people were still being infected with smallpox every year while the chart on the reported cases below indicates only 132,000 for that same year.17
The reasons and extent of discrepancies between reported and estimated cases are discussed in our section on Data Quality.
The chart shows global case numbers (as shown in the section above) disaggregated by world region, extending to 1977, the year of the last case globally.
Even though absolute numbers are almost certainly far too low (as explained above and in our section on Data Quality), it can be seen that in relative terms, South Asia had by far the highest number of smallpox cases. This was primarily driven by incidence in India: in 1973, for instance, in a state that had reported approximately 500 cases a week, the WHO search team found 10,000 cases.18
Eradication of smallpox
The last variola major infection was recorded in Bangladesh in October 1975, and the last variola minor infection occurred two years later in Merka, Somalia, on October 26th, 1977. During the following two years, WHO teams searched the African continent for further smallpox cases among those rash-like symptoms (which is a symptom of numerous other diseases). They found no further cases.
In 1978, a laboratory accident in the United Kingdom occurred where a variola virus sample was spread through the university laboratory’s ventilation system, infecting two people and killing one.19
The world map shows the year in which each country recorded the last endemic case of smallpox. Europe, North America and Australia managed to eliminate smallpox relatively early, most by the 1940s (predating the WHO’s Intensified Smallpox Eradication Program, which was launched in 1966). Countries across Sub-Saharan Africa, Latin America and Asia eliminated smallpox several decades later in the 1960s and 70s.
In May 1980, the World Health Assembly, the governing body of the World Health Organization, officially certified the global elimination of smallpox, the first ever eradication of a disease in human history. It further “recommended that all countries cease vaccination, all laboratories should destroy their remaining stocks or transfer them to” two certified high security laboratories in Moscow (State Research Center of Virology and Biotechnology) or the Centers for Disease Control and Prevention (CDC) in Atlanta.20
These are the only two known places that still hold samples of the variola viruses for research purposes.
Variolation
Variolation (sometimes also inoculation), refers to the deliberate transmission of viral matter.
Before the year 1000, Indians and the Chinese had already observed that contraction of smallpox protected children against any future outbreaks of the disease. As a consequence they developed a procedure that involved the nasal inhalation of dried smallpox scabs by three-year-olds.21
Another commonly practiced technique (whose geographic and temporal origin are unknown) encompassed the injection of the liquid found inside the pustules of a smallpox patient underneath the skin of a healthy person. This would usually result in a milder infection of smallpox after which the person was immune against the disease. Both practices became known as variolation (inoculation) techniques.
The disadvantage of variolation, however, was that during the course of the mild infection the person became a carrier of the disease and could infect other people. Additionally, it was difficult to control the severeness of the infection which sometimes developed into a full-blown smallpox case that could lead to the person’s death.22
This meant that the practice usually reduced the severeness of an infection and the likelihood of deaths but that it would never lead to eliminating the virus. If anything, it helped to spread the virus in a population even further and thereby encouraged its survival.
A British ambassador’s wife, Lady Mary Wortley Montague (1689-1762) was the force that pushed for government-mandated variolation in England. She herself had suffered a smallpox infection and lost her younger brother to the disease at the age of 26. She first learned about variolation when she arrived in Istanbul in 1717, where variolation was commonly practiced. She later had the embassy inoculate her two children.
News spread among the royal family and after following trials Maitland successfully inoculated the two daughters of the Princess of Wales in 1722. Thereafter, variolation became a common practice in Great Britain and became known in other European countries. It became an even more established practice when the French King Louis XV died of smallpox in May of 1776 and his successor and grandson Louis XVI was inoculated with the variola virus one month later.
Vaccine against smallpox
At the end of the 18th century British surgeon and physician Edward Jenner (1749-1823) pioneered the first ever vaccination against an infectious disease. He himself had been inoculated with smallpox at the age of 8 and later as a surgeon, variolation was part of his work.23 He observed that people who had suffered from cowpox would subsequently have a very mild, if at all visible reaction to the smallpox variolation. At the time unknowingly, he had discovered that the cowpox and variola viruses were members of the same orthopoxvirus family.
He hypothesized that variolation using the cowpox virus would protect children against smallpox as well. Since cowpox infections were much milder and never fatal, this would eliminate the problem of variolated children being carriers of smallpox and sometimes dying of the virus developing into a full-blown infection. On top of protection against the symptoms, it could reduce the stock of humans that the variola virus needed for survival and brought elimination and eventually eradication of smallpox into the realm of possibility.
In May 1796, Jenner inoculated a boy with cowpox, and then a few months later with the smallpox virus. When the boy did not develop any smallpox symptoms in response to being variolated, his hypothesis of the cowpox offering protection from smallpox was confirmed motivating his further research trials.
Initially, Jenner faced major barriers to spreading the word about his discovery. When he submitted a paper outlining his findings to the journal Philosophical Transactions edited by the Royal Society, it was rejected. They even advised him not to pursue his ideas any further, pointing to the detrimental impact on his career and reputation. Undeterred, he published his work with an increased number of trials at his own expense two years later (in 1798). He also went on to convince colleagues and supply them with vaccines in other British cities of his new procedure that became known as vaccination (derived from the Latin word for cow, vacca).
By 1802, the British Parliament did acknowledge his important contribution and awarded him £30,000. Meanwhile, vaccination had spread to most of Europe and New England.24
His 1798 publication Inquiry into the Variolae vaccinae known as the Cow Pox had been translated into German, French, Spanish, Dutch, Italian, and Latin within three years. US President Thomas Jefferson figured importantly in the widespread application of vaccination throughout the United States and in 1806, he thanked Edward Jenner in a letter for his discovery and famously predicted “Future generations will know by history only that the loathsome smallpox existed and by you has been extirpated.”25
The dramatic decline in smallpox fatalities in response to Jenner’s vaccine can be traced in the chart, which shows the number of deaths due to smallpox as a share of all deaths in London from 1629 to 1902. Before the introduction of a smallpox vaccine in 1796, on average 7.6% (1-in-13) of all deaths were caused by smallpox. Following introduction of the vaccine, we see a clear decline in smallpox deaths.
Smallpox Eradication Program
It was only with the establishment of the World Health Organization (WHO) in the aftermath of World War II that international quality standards for the production of smallpox vaccines were introduced. This shifted the fight against smallpox from a national to international agenda. It was also the first time that global data collection on the prevalence of smallpox was undertaken.
By 1959, the World Health Assembly, the governing body of the World Health Organization (WHO) had passed a resolution to eradicate smallpox globally. It was not until 1966, however, that the WHO provided the ‘Intensified Smallpox Eradication Program’ with funding to increase efforts for smallpox eradication.
By 1966, the number of infections of smallpox had already substantially been reduced by national governments’ efforts. Nonetheless, skepticism about the feasibility of eradication prevailed and the WHO lacked experience in administering projects that required both technical and material support, as well as coordination across countries. Furthermore, the funding provided to the Intensified Smallpox Eradication Programme was insufficient to meet global needs, resulting mostly in vaccine shortages.26
Further still, continued globalization and growth of international air travel resulted in the continual re-introduction of the disease into countries that had previously managed to eliminate smallpox.
Overcoming the last mile problem: ring vaccination
Smallpox’s eradication was greatly spurred by making use of the fact that smallpox transmission occurs via air droplets. Initially, the WHO had pursued a strategy of mass vaccination which attempted to vaccinate as many people as possible, hoping that herd immunity (explained in our vaccine entry) would protect the whole population. Soon, however, vaccination efforts were targeted locally around smallpox cases as smallpox was transmitted by sick patients’ air droplets. This is known as the ring vaccination principle.
People who had been in direct contact with a smallpox patient over the last two weeks were quarantined and vaccinated. The downside of such an approach was that the virus could spread easily if it was re-introduced from overseas. This was the case in Bangladesh, for example, which had previously eliminated smallpox until 1972 when it was brought back from across its border with India.27
Despite the risk of re-introductions, ring vaccination greatly reduced the cost of the eradication campaign. The number of administered vaccines dropped and smallpox was increasingly brought under control. Regional elimination came within reach.28
One of the last strongholds of the variola virus was India. While 57.7 percent of global reported smallpox cases were reported in India in 1973, this increased to 86.1 percent in 1974.29 One major push in vaccination campaigns, however, successfully drove down the number of infections to zero in India in 1976.
Impact on life expectancy
Did smallpox variolation and vaccination against smallpox have a notable impact on life expectancy?
Many have made the claim that inoculation against smallpox was one of the first measures that had a positive effect on life expectancy. Angus Deaton (2013) makes this claim based on a book by Razzell (1977), which reviews existing birth, baptism and burial records in various counties of 18th century Britain.30 31 Whilst some anecdotal evidence suggests smallpox deaths declined over the course of the 18th century, we cannot be sure that the spread of inoculation practices were the cause of that decline. Furthermore, the local communities for which records were available may not have been representative of Great Britain as a whole. Such evidence therefore seems insufficient to show a causation relationship between inoculation and increases in life expectancy.
It is hard to prove such claims because of the lack of and low quality of data on both life expectancy and smallpox cases/deaths prior to the invention of Jenner’s vaccine in 1796. Whilst we have presented data on smallpox deaths in London dating back to 1629, we only know the aggregate life expectancy of Great Britain (rather than London specifically) over this period. It’s unlikely that London’s smallpox deaths are nationally representative which means that the direct comparison is not possible.
When comparing these charts on London smallpox deaths and British life expectancy we see that neither smallpox deaths or life expectancy dramatically deviated from their averages following the wider adoption of variolation in 1722.
But can we say something about the impact of Jenner’s vaccination on life expectancy? The high case fatality rate of approximately 30 percent (for the variola major virus strand) meant that smallpox shortened the lives of many. Since the virus predominantly affected children during endemic periods, smallpox deaths are likely to have had a disproportionate impact on average life expectancy.
The chart visualizes Sweden’s life expectancy (in red) and deaths from smallpox (in blue) from 1774 to 1900. Large-scale smallpox outbreaks were documented for the years 1779, 1784, 1789, 1795 and 1800. These years exactly coincide with sharp declines in life expectancy, implying that smallpox endemicity did have a substantial effect on life expectancy. Furthermore, while the available data did not show a clear decline in smallpox deaths after the introduction of inoculation in Britain, they do show dramatic declines in mortality in London as well as in Sweden (below) from 1800 onwards. Once smallpox mortality fell at the turn of the eighteenth to nineteenth century, life expectancy in Sweden for the first time was put on an upwards trending trajectory.
Overall, the impact of inoculation on life expectancy remains uncertain. Jenner’s vaccine appears to have had a notable impact on increased life expectancy but this, to our knowledge, has not been studied in significant detail.32
Costs of smallpox and its eradication
By the time the World Health Organization launched the Intensified Smallpox Eradication Program in 1967 many countries, most of them high income countries, had already eliminated smallpox. Therefore, the true cost of eradicating smallpox will never be known as individual country programs reach back to before records of public health expenditure existed. Nonetheless, the Intensified Smallpox Eradication Program has been estimated to have cost $300 million in total from 1967 to 197733 with one-third of the funding provided by international donors and the remaining two-thirds financed by endemic country governments.34
Beyond direct program costs, smallpox incurred much higher indirect costs in the form of foregone economic performance. It has been estimated that smallpox cost low-to-middle income countries more than $1 billion per year at the beginning of the Intensified Smallpox Eradication Program in 1967, with more than $20 million dedicated to the care of infected patients.35
Industrialized countries incurred much lower costs: $350 million in 1968 which included vaccination programs and absence from work costs.36
Overall, the Center for Global Development37 estimated that direct and indirect costs of smallpox cost the world approximately $1.35 billion in the late 1960s.
Following its eradication, countries now do not have to spend money on vaccine development and administration. Estimates on the savings from forgone costs thanks to the eradication of smallpox exist, but we are not aware of estimates that we would consider reliable.38
Lives saved from smallpox eradication
To date the eradication of smallpox saved millions of lives. It is impossible to know very exactly how many people would have died of smallpox since 1980 if scientists had not developed the vaccine, but reasonable estimates are in the range of around 5 million lives per year, which implies that between 1980 and 2018 around 150 to 200 million lives have been saved.39
Epidemiological definitions/context
The origin of the naming of smallpox and the variola virus
The name of smallpox originates from a common confusion with syphilis in 15th century France. The diseases shared similar symptoms (rashes) even though syphilis was caused by spirochaete bacteria and smallpox by the variola virus. Syphilis had already been known as variola, so smallpox became known as la petite vérole. Petite is French for small so the disease became known as smallpox in English.
The name of the variola virus, in turn, can be derived from the Latin words varus (pimple) or varius (changing color) which derive from smallpox’s symptoms described above.40
The variola virus family tree
The variola virus is a member of the so-called orthopoxvirus family, whose other members are the vaccinia, cowpox and monkeypox viruses.41
This is important as Jenner’s vaccine used the cowpox virus, a much milder and not lethal disease, to protect humans against smallpox. The variola virus is the family’s only virus that exclusively infects humans.
The variola virus consists of two strands, known as the variola major and variola minor viruses. Infections of the variola major strand led to a patient’s death in approximately 30% of cases, whereas the variola minor virus proved lethal in only less 1% of infections.42
Eradication is the “permanent reduction to zero of the worldwide incidence of infection caused by a specific agent as a result of deliberate efforts”.43
Elimination refers to the “reduction to zero of the incidence of infection caused by a specific agent in a defined geographic area as a result of deliberate efforts.” A disease can be eliminated from a specific region without being eradicated.44
Infectious Diseases are “disease[s] caused by the entrance into the body of organisms (as bacteria, protozoans, fungi, or viruses) which grow and multiply there”.45
Variolation refers to the deliberate transmission of viral matter, for example by inserting material from an infected person’s skin underneath a healthy person’s skin.46
Endemic refers to the constant presence […] of a disease in a population within a geographic area.47
Endemic vs. non-endemic populations
The severity and most common age group for smallpox infections was dependent on whether the virus was endemic in a population. If a population had never been exposed to smallpox before, all age groups were vulnerable to infection, meaning outbreaks led to high case and death rates across the population. McMillan (2016)48
terms this a ‘virgin soil epidemic’, i.e. when a disease touches “soil” it has never touched before. The most prominent example of smallpox attacking an unprotected and never-exposed population in history is the introduction of the variola virus in North America by British colonialists. Data on the deaths of Native American tribes suffered were unfortunately not collected at the time but available sources agree that tribes were substantially decimated.49
Regularity and severity
In an endemic population, on the other hand, smallpox outbreaks with large numbers of cases and deaths usually occurred only every two to four years. In the periods between large outbreaks, the disease would persist at lower levels of incidence (with lower numbers of cases and deaths).
Such a pattern is common among viral diseases in an endemic population: by the time the virus had infected a population, an outbreak either engendered immunity or death, so a renewed outbreak in a subsequent year would infect fewer people.50
These cyclical outbreaks can be observed in the volatile pattern of the smallpox share in London deaths and also the smallpox death rates across Europe.
Age profile of patients
Smallpox could infect people of any age. However, when the virus was endemic in a society (uninterrupted transmission without depending on re-introduction from elsewhere), it mainly infected children. Adults in an endemic population would have been infected with the virus at an earlier stage in their lives already and since the only two possible outcomes of an infection were death or survival and life-long immunity, the virus could only infect and be transmitted by individuals that had never been exposed before: children.
In 17th century Britain, this led to children not being considered full members of the family until they had survived their smallpox infection. At the time, the British had not yet come up with a protection against smallpox so children were almost guaranteed to fall prey to an infection and families could do nothing but watch the infection run its course and hope the child would survive.51
Why are there differences between reported and estimated cases?
Three main reasons are responsible for the huge differences between reported and the estimated (thought to be closer to the truth) number of cases and deaths due to smallpox. First, many infections and deaths were not recorded simply because the monitoring public health system was dysfunctional and that was predominantly the case in developing countries where the disease burden was highest. Fenner et al. (1988) write: “It is clear that the reporting of cases of smallpox was the most efficient in countries in which the health services were well developed, which was usually where the disease was least common. It was very inefficient elsewhere.”52
Second, classifying deaths posed another challenge. For instance if smallpox patients had already been suffering from pneumonia or even just a flu when becoming infected with smallpox and then died, it is unclear whether smallpox or pneumonia or the flu were the cause of death. Had a patient survived the smallpox infection if (s)he had not already been weakened by another disease, this creates a major challenge in classifying the cause of deaths which is likely to have further diminished the number of smallpox cases and deaths actually reported and recorded.
Third, some anecdotes suggest that some smallpox outbreaks were deliberately kept secret.53
Razzell (1977) writes in his book about British market towns: “Many tradesmen in market towns may have suppressed information about smallpox in their families and certainly the townspeople as a whole were very anxious to avoid advertising the presence of smallpox in their own town so as to avoid frightening country people from the surrounding area – there are many examples of markets being ruined for more than a year because of the presence of smallpox.”54
Extent of reporting discrepancy
The World Health Assembly was aware of the underreporting and therefore attempted to correct the number of reported smallpox cases upward for the years 1959 to 1966, just before the Intensified Smallpox Eradication Program was launched. The chart illustrates that the corrections were highest for 1965, where the originally reported smallpox cases only amounted to 64,000 cases which was corrected to almost double its value, 112,000 cases.
Many sources suggest, however, that even these corrections were small in comparison to what the actual extent of smallpox’s disease burden was. Fenner et al. (1988) write “it is not unreasonable to regard the official figures reported to WHO as representing only 1-2 percent of the true incidence – probably nearer 1 percent for the years before the initiation of the global eradication programme. In the early 1950s, 150 years after the introduction of vaccination, there were probably some 50 million cases of smallpox in the world each year, a figure which had fallen to perhaps 10-15 million by 1967.”55
These figures are also mentioned in the final report by the WHO that confirmed smallpox’s eradication, along with the disease still causing approximately 2 million deaths in 1967.56
Henderson (1976) adds that the global cases numbers reported to the WHO in 1967 probably were the number of infections taking place in northern Nigeria alone.57
In 1973, the World Health Organization conducted a thorough search for smallpox cases in line with its ring vaccination strategy in India: in a state that had reported approximately 500 cases a week the search team found 10,000 cases.58
- Data: Global number of smallpox cases
- Geographical coverage: Global (total)
- Time span: 1920-2016
- Available at: Link under the data tab at the right on the Earth Policy Institute’s website here.
- Data: The year of the last recorded smallpox case and the reported number of smallpox cases
- Geographical coverage: Global (by country)
- Time span: Year of the last recorded smallpox case: 1910-1977
Reported number of smallpox cases: 1886-1966 - Available at: Chapter 8 of Fenner, F., Henderson, D., Arita, I., Jezek, Z., & Ladnyi, I. (1988). Smallpox and its eradication. Geneva: World Health Organization. Fully available for download here.
- Data: The reported number of smallpox cases
- Geographical coverage: Global (by country)
- Time span: 1967-1977
- Available at: Archived Weekly Epidemiological Records available on the WHO website but the links to the relevant decades at the bottom of the list are unfortunately dysfunctional. Therefore, the search function at the top right was used and search times such as “Weekly Epidemiological Record 1970” were used. Direct links to the individual volumes used for graphs on this entry can be found under the “Sources” tab of the graph The number of reported smallpox cases.
- Data: The number of deaths caused by smallpox as a share of all deaths
- Geographical coverage: London
- Time span: 1629-1902
- Available at: The Guy (1882) paper is available on JSTOR here. For detailed information on which data sources we used in addition to Guy (1882), click on the Sources tab at the bottom of our graph for individual years’ references.
- Data: The number of smallpox deaths per 1,000 (living) population
- Geographical coverage: Austria, Belgium, England, Netherlands, Prussia, Scotland, Sweden
- Time span: 1774-1900
- Available at: Edwardes (1902) A concise history of small-pox and vaccination in Europe. H.K. Lewis. Available online here.
- Description: This is an animated video illustrating the history of smallpox from its spread and Edward Jenner’s discovery all the way to its eradication.
- Date of publication: October 2013
- Available at: https://ed.ted.com/lessons/how-we-conquered-the-deadly-smallpox-virus-simona-zompi#watch.
- Description: This is an in-depth historical account of everything you ever wanted to know about the disease and its history.
- Date of publication: 19 April 2013
- Available at: Partially on Google Books.
- Description: This is an approachable summary of infectious diseases with particularly high disease burdens, with chapter two dedicated to smallpox
- Date of publication: 2016
- Available at: Google Books in parts.
- Description: This book takes a deep dive into the history and potential future threat of smallpox being used as a biological weapon.
- Date of publication: 2001
- Available at: Google Books in parts.