1.6 million people died because of diarrheal diseases in 2017. Diarrheal diseases are among the leading causes of death globally. In this entry we look at the burden of diarrheal diseases and what can we do to reduce it.
Summary
- Diarrheal diseases were the third leading cause of death of children younger than 5 in 2017 and are becoming an increasing burden in people aged 70 and over.
- The highest mortality from diarrheal diseases is in Sub-Saharan Africa and South Asia.
- Most childhood cases of diarrhea are caused by rotavirus and most diarrhea cases in older people are caused by shigella bacteria.
- The highest risk factors for development of diarrheal diseases are unsafe drinking water and poor sanitation. For children child growth failure and vitamin A deficiency are also important.
- Rotavirus vaccines are effective at preventing diarrhea in children and have saved more than 128,000 lives of children in 2016.
- Oral rehydration therapy is a low-tech solution to treat people with diarrhea. It has saved more than 70 million lives since its first use in 1960s.
Diarrheal diseases are one of the biggest killers of children worldwide
In 2017, almost 1.6 million people died from diarrheal diseases globally.
This is more than all deaths from all ‘intentional injuries’ combined in the same year: almost 800,000 died from suicide, 405,000 from homicide, 130,000 in conflict, and 26,500 from terrorism – in total 1,355,000.1
As the visualization shows, one-third of all who died from diarrheal diseases were children under five years old. For most of the past three decades under-5s have accounted for the majority of deaths from diarrheal diseases – back in 1990 it killed 1.7 million children.
Diarrheal disease was the cause of every tenth child’s death in 2017 – more than half a million of the 5.4 million children that died in 2017 died from diarrheal disease.
Diarrheal diseases are the third leading cause of child mortality globally, falling just behind pneumonia and preterm birth complications.
Diarrheal diseases death rates
In the map we see death rates from diarrheal disease, expressed as the number of deaths per year per 100,000 individuals.
These rates have been age-standardized to adjust for differences in the age structure of a population between countries and changes over time. This therefore allows us to make comparisons between countries and over time that are not affected by changes of the age-structure.
Overall, we see the highest death rates in Sub-Saharan Africa and South Asia, where rates typically range from 50 to 150 per 100,000. In the Central African Republic and Chad rates are estimated to be over 150 per 100,000.
Across most of the rest of the world, rates are below 5 per 100,000 and in some cases below 1 per 100,000.
Moving the time slider back to 1990 shows that the death rates were much higher back then.
Where are children dying from diarrheal diseases?
The death rate from diarrheal diseases is highest in the world’s poorest countries: this chart shows the relationship between the death rate from diarrheal diseases and the country’s average income.
The death rate from diarrheal diseases in many of the poorest countries is higher than 100 annual deaths per 100,000 children. In those countries with the worst health – including Madagascar, Chad and the Central African Republic – the rate is higher than 300 per 100,000.
In high-income countries the death rate is very low. In many European countries, but also some rich Asian countries the rate is below 1 per 100,000 per year.
At lower levels of income risk factors for diarrheal diseases such as lack of access to clean water, rotavirus vaccine availability, undernutrition, stunting and others are the most prevalent.2
Understanding the cause of disease is important so that we can set our priorities on the interventions and treatments that save most lives.
What causes diarrheal disease in children?
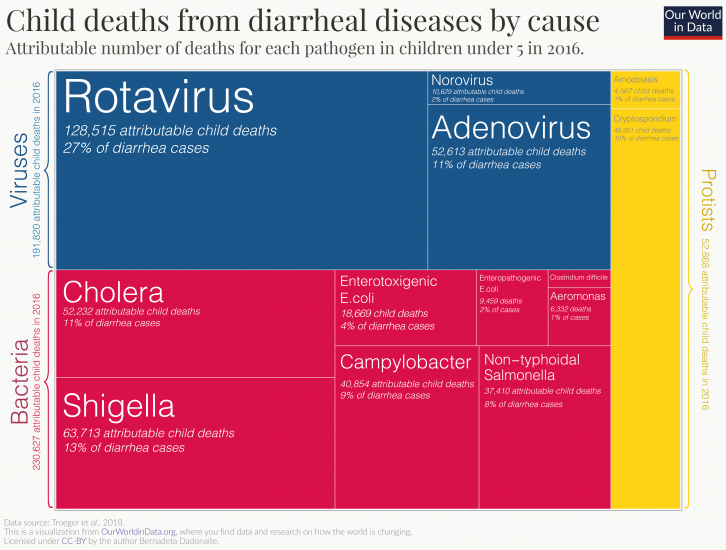
Diarrheal diseases are caused primarily by viral and bacterial pathogens. The visualization shows the major pathogens responsible for diarrhea in children; the area of each box corresponds to the number of deaths from diarrhea in 2016 that can be attributed to each pathogen.
While bacterial pathogens (shown in red) are the major group of organisms responsible for diarrheal diseases, rotavirus is the single largest causative agent.3
What causes diarrheal disease in people aged 70 and over?
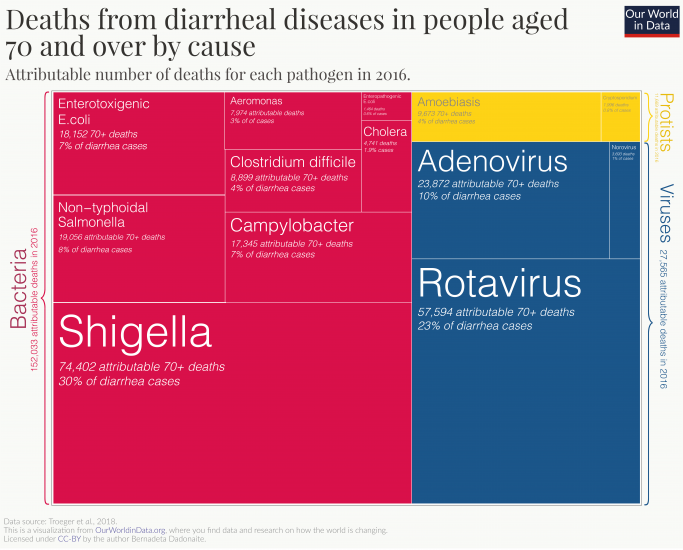
The majority of cases of diarrhea in people aged 70 and over are caused by bacterial pathogens. The pathogen responsible for most deaths from diarrhea in this age group is shigella. As the visualization shows, shigella bacteria were responsible for 30% of attributable diarrheal deaths in 2016. Unlike the for the rotavirus, no vaccine is yet available for shigella and currently antibiotic-treatment is prescribed for suspected cases.4
While rotavirus does infect adults, the infection is usually less severe than in children.5
Risk factors increase the chances that a person will develop a disease. Understanding the importance of different risk factors for different diseases allows us to target the ones that will make the most impact in reducing the number of deaths.
For diarrheal diseases, interventions that improve water, sanitation and hygiene conditions are the best way to prevent diarrheal diseases across all age groups.
Why are children still dying from diarrhea?
There are two main reasons why the number of children dying from diarrhea is still so large – the prevalence of diarrhea-associated risk factors and the lack of access to essential treatment.
The figure shows the number of deaths associated with the major risks factors for diarrheal diseases: unsafe drinking water, poor sanitation and malnutrition are responsible for the largest portion of deaths.
Since 1990 we have made a lot of progress in reducing these major risks; you can read more in our research entries on Hunger and Undernourishment, Extreme Poverty and Water Use and Sanitation. But continued progress is still needed.
In addition to reducing exposure to risks factors, increasing access to oral rehydration therapy (ORT), therapeutic zinc use and the coverage of rotavirus vaccines were all shown to be essential for reducing the burden of diarrheal diseases in children.6
Risk factors for diarrheal diseases in people aged 70 and over
This chart shows that unsafe drinking water is the greatest risk factor for people who are 70 years and older to develop diarrheal disease.
The number of people in this age group dying from diarrheal diseases due to the poor water, sanitation and hygiene conditions has increased in the past decades. This is to a large degree a reflection of population aging and the increased number of people aged 70 and over in the population: The death rates – which are unaffected by population changes – due to these risk factors have fallen. In 1990 the death rate due to unsafe water use was 174 individuals per 100,000, today that rate is 109 per 100,000.
The first widely-used rotavirus vaccine was approved in the United States in 2006. Today, there are four oral rotavirus vaccines recommended for use by the World Health Organisation (WHO): Rotarix, RotaTeq, RotaSiil, and Rotavac.7
Rotarix and RotaTeq are the most widely used and both have shown good efficacy against rotavirus infections in clinical trials.89
Since the use of rotavirus vaccines have been approved, they have had a notable impact on the reduction of rotavirus-related deaths. According to a study published in 2018, the use of rotavirus vaccines prevented approximately 28,900 child deaths globally in 2016. However, as the chart shows, full vaccine use – that is a 100% coverage globally – could have prevented an additional 83,200 deaths.10 This means that, even at the current rates of efficacy, 53% of all deaths in children under-5 from rotavirus in 2016 could have been avoided by full vaccine coverage.
In addition to saving lives, the rotavirus vaccine also reduces the burden on healthcare systems. Between 2008 and 2016 the introduction of the rotavirus vaccine has reduced the number of diarrhea-related hospital admissions on average by 40%.11
If there is so much scope for saving more children’s lives, what is the reason that these children are still dying?
There are two key barriers to achieving the full potential of the rotavirus vaccine: immunization rates, and the efficacy of the vaccine in specific regions.
According to the WHO, by the end of 2018, 101 countries were using the rotavirus vaccine. The major drivers for the introduction of the vaccine are the burden of diarrheal diseases, the availability of funding, and a favourable political climate for vaccines.12
The vaccine is only given to children – it’s recommended that the vaccination should be initiated 15 weeks after birth and finished by the 32nd week. However, the global coverage is still very low: it is estimated that just 35% of under one-year-olds were vaccinated in 2018.13
The map shows the WHO estimates on the share of one-year olds who received the full recommended dosage of the vaccine (two immunizations for Rotarix vaccine or three immunizations for RotaTeq vaccine). For many countries where data coverage is low, it’s expected that the share of infants receiving the vaccine is very low. Some countries however did see rapid increases in rates of immunization. In a period of only a few years countries including Sudan, Malawi and Gambia have increased immunisation rates from below 10% to 80-95% – click on the country to see the change over time.
Since most rotavirus cases occur in Sub-Saharan Africa where mortality from rotavirus infection is also the highest, it is essential to increase and maintain high immunisation coverage in this region. However, in addition to delivering the vaccine for those who need it, we also need to work on improving its efficacy.
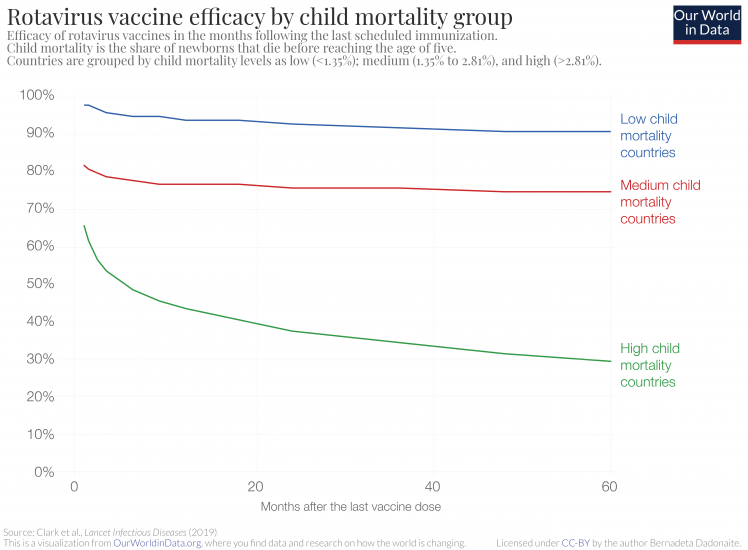
Vaccine efficacy for the rotavirus vaccine is defined as the percentage reduction of the rate of diarrhea incidences in vaccinated versus unvaccinated groups of children. It is well established that the efficacy of the rotavirus vaccine is not the same across all countries — in countries with high child mortality rates the vaccine shows much lower efficacy.14
The chart is from a recent study by Clark et al., which looked at how the efficacy of live oral rotavirus vaccines changes in different countries following vaccination. The chart shows that in countries with high child mortality rates, not only is the immediate vaccine efficacy lower – 98% in low child mortality countries versus 66% in high child mortality countries – but also the vaccine efficacy decreases faster in high child mortality countries over time.15
Five years after vaccination, the rotavirus vaccine reduces the chances of getting diarrhea by 90% in low child mortality countries and only by 30% in high mortality countries.
The table shows how good the rotavirus vaccine is at preventing severe diarrhea and reducing hospitalization due to diarrhea in children under-5 in different regions.16
In high-income countries, rotavirus vaccination has been shown to reduce the cases of severe rotavirus diarrhea by 91% and hospitalization by 94%. In Eastern Asia and Latin America, the effectiveness rates are lower but still high – preventing 88% and 80% of severe diarrhea cases, respectively. However, effectiveness in South Asia and Sub-Saharan Africa is significantly lower, only reducing severe diarrhea in around half of the cases.
The reasons for different responses to the vaccine are not entirely clear.17 18
It is likely that the gut responses to the oral rotavirus vaccines in children in lower-income countries are different. This may be due to a variety of causes, including micronutrient deficiencies, pre-vaccination exposure to certain pathogens, and the presence of chronic conditions such as malaria or HIV. Overall, the poor gut response to the live vaccine means the efficacy of the vaccine is reduced. Taking all of the above mentioned points into account, there are several interventions that could increase the benefits of the rotavirus vaccine even further. In addition to increasing the vaccine coverage, improving nutritional health (of both infants and mothers) and improving hygiene and sanitation conditions (to lower the prevalence of damaging pathogens) could have positive effects on the vaccine’s efficacy.
We are still at quite an early stage of the rotavirus vaccine use. Although the vaccine has brought huge benefits already, it could go even further. Improving vaccination coverage, particularly across Sub-Saharan Africa and South Asia is key to continued reduction of childhood deaths from diarrhea. Even at moderate levels of vaccine efficacy, a significant number of additional additional child deaths could be prevented every year. The bar chart above that shows the number of preventable deaths illustrates the potential for extended vaccine coverage to save many more lives. And this is already taking into account the regional differences in the vaccine’s effectiveness.
In addition to increased coverage, improving the effectiveness of the vaccine would go even further in tackling one of the leading causes of death.
| Outcome | Region | Vaccine effectivness |
|---|---|---|
| Severe rotavirus diarrhea | Developed | 91% |
| Eastern Asia and Southeast Asia | 88% | |
| Latin America and Caribbean | 80% | |
| Southern Asia | 50% | |
| Sub-Saharan Africa | 46% | |
| Hospitalization due to rotavirus infection | Developed | 94% |
| Eastern Asia and Southeast Asia | 94% | |
| Latin America and Caribbean | 84% | |
| Sub-Saharan Africa | 58% |
Oral rehydration therapy is a very simple and cheap treatment which save many lives every day, but it took humanity surprisingly long to realize it.
Here is what we know:
- Over recent decades the number of children dying from diarrheal diseases has fallen very substantially (by two-thirds since 1990).
- Oral rehydration therapy (ORT) is a large part of the success story. It is estimated that it saved around 70 million lives since its introduction in the late 1970s.
- ORT is a simple, cheap and effective treatment for a major public health problem.
- Still close to half a million children die every year from diarrheal diseases.
- Increasing the coverage of ORT globally has the potential to save many more lives.
In recent decades the world has made significant progress in reducing the number of deaths caused by diarrheal diseases. 2.6 million people died from diarrheal diseases back in 1990. Since then, the annual number of deaths from diarrheal diseases fell by around one million.
Progress against diarrheal deaths among children has been even more substantial: deaths of children under 5 have fallen by two-thirds since 1990.19
In this post I want to focus on one intervention that has played a large role in reducing child deaths from diarrheal disease across the world and that has the potential to save many more lives in the future: oral rehydration therapy.
Diarrhea can lead to life-threatening dehydration and therefore, an effective treatment needs to target the loss of fluids. Oral rehydration therapy (ORT, also referred to as ORS) is one of the most common treatments used to prevent dehydration caused by diarrhea.20
ORT is an incredibly simple therapy: a mixture of water, salt and sugar. It can be administered orally, without the need for special medical assistance. Simple as it may seem, the medical journal The Lancet has called ORT “the most important medical advance of the 20th century”.21
You can read more about the biological mechanism of how ORT works here.
When it comes to “the most important medical advances” and life-saving interventions, we often think about expensive drugs and complicated surgeries that were discovered and perfected in sophisticated laboratories. ORT defies these expectations. Not only is it low-tech and cheap (only around 0.50$ per treatment course), but it was also developed far away from the world’s leading hospitals, under often challenging circumstances.
The early hospital trials for ORT in the late 1960s were performed by Drs Richard Cash and David Nalin in Dacca, in today’s Bangladesh. The most common treatment for diarrhea at the time was the much more expensive intravenous rehydration therapy (IVT), which involved the administration of saline solution intravenously in hospital settings. While IVT was an effective treatment, Cash and Nalin recognized the need for an alternative treatment because the people most affected by diarrheal disease were those who did not have access to clinical centers where IVT was available. In addition, the possibilities of scaling-up IVT use during large outbreaks of diseases – such as cholera epidemics – were limited.
In the late 1960s Cash and Nalin conducted a number of small clinical trials during cholera epidemics in the region, which showed the promise of ORT.22 However, the most significant proof of ORT effectiveness came from desperate circumstances during the Indo-Pakistani War in 1971.23 The conditions of war, complicated by the monsoon season, displaced millions of people into refugee camps, which ultimately led to a disastrous cholera outbreak. Early during the outbreak almost 30% of the afflicted patients died due to the shortage of the IVT therapy. Pressed by the disastrous circumstances, Dr Dilip Mahalanabis decided to start providing bags of salt and sugar dissolved in water to the people in the camp. The decision by Dr Mahalanabis proved to be the right one: in just a few months the case-fatality ratio from cholera and cholera-like diarrheal diseases fell below 4% among the people treated with ORT, as compared with the 30% ratio observed previously. This success was a major stepping stone for wider adoption of ORT.24
While ORT is a simple, low-tech solution for the treatment of diarrhea – a major public health issue – it took many years for its use to be accepted. It wasn’t until 1978 that the World Health Organization (WHO) created the diarrheal disease control program that has helped to popularise the use of ORT worldwide.25 To put this into perspective – we only adopted the use of ORT more than a decade after we landed on the Moon.
There are many reasons why the uptake and recognition of ORT by richer countries was slow. Western doctors were skeptical of adopting treatments tested in developing countries and considered these to be of a lower standard.26 The idea that drinking a simple water, sugar, and salt solution, was just as good of a treatment as a “sophisticated” intravenous drip seemed radical at the time. And, even today, ORT treatment seems counterintuitive, because, while it reduces the likelihood of death and speeds up recovery, it does not actually prevent or stop diarrhea.
How many lives has ORT saved? The exact number is in some ways impossible to know because many other interventions and treatments have contributed to the decreasing number of deaths from diarrheal diseases. However, the incredible decline in deaths from diarrheal diseases in children in the last two decades of the 20th century (from around 4.8 million annual deaths in 1980 to 1.2 million deaths in 2000) has coincided with an expanded global use of ORT. A number of researchers have suggested that the dramatic decline was not just a coincidence but directly caused by the increased ORT use.27 Twelve years ago Fontaine, Garner, and Bhan estimated that more than 50 million children have been saved by ORT between 1982 and 2007 – that is on average of 2 million lives a year.28 Based on these estimates the number of children saved from 1982 until 2019 by ORT could be more than 70 million. Whatever the exact number of lives saved is, it would not be an overstatement to say that many adults would not be alive today if not for the discovery of ORT.
ORT could still go further
We are not benefiting from the full potential of ORT. The main reason for this is that it is not as widely used as it could be. As the map shows, the coverage of ORT is still low.
According to data from UNICEF, on average only 44% of children with diarrhea receive ORT (you can view this data on the Chart tab in the interactive visualization).29 In some countries the coverage is very low, at less than 1-in-5.
Of course, one has to ask: does every child with diarrhea need ORT? According to the current WHO guidelines, the need for ORT should be determined based on the degree of child’s dehydration.30 If a child has diarrhea but is not dehydrated, home treatment with fluids that contain salt, such as rice water or chicken stock, is sufficient. If a packet of ORT salts is available it can be used but is not a necessary treatment. If a child has moderate or severe dehydration, ORT should be given. According to a study conducted in 2012, 35.2% of all diarrheal cases in children were classified as moderate or severe, suggesting that at least a third of diarrheal instances should have been treated with ORT: in 2012 that accounted for 588 million diarrheal episodes.31
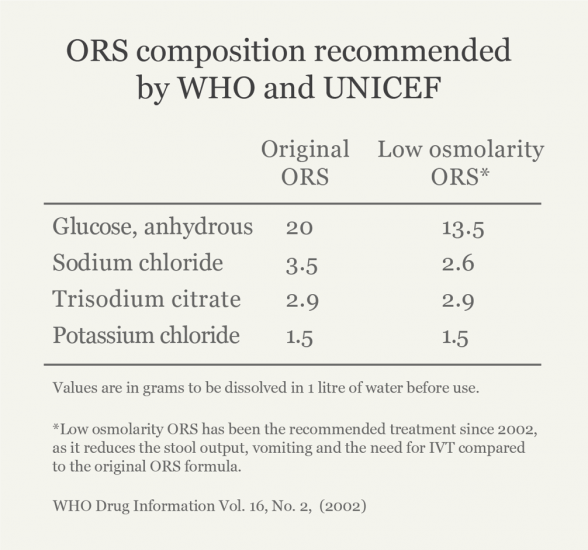
Greater promotion and education about the use of ORT in healthcare facilities and community centers could potentially increase ORT coverage. In addition to increasing coverage, more lives could also potentially be saved by switching to a more effective ‘low osmolarity’ ORT formulation, that is currently recommended by the WHO.32
How many more lives could ORT save?
An analysis from 2010 by Munos et al. in the International Journal of Epidemiology is the most widely cited study that provides estimates for the number of potential lives a wider use of ORT could save. The study looked at all the available literature on ORT at the time and suggested that, if every child who needs ORT would receive it, 93% of child deaths caused by diarrhea could be prevented.33
This implies a huge potential for ORT.
We should be somewhat cautious, however. The study is the only currently available published research review that measures the effectiveness of ORT. And because there are only a few studies that have looked at how providing ORT directly affects child mortality, the 93% figure was determined based on a very small sample. Furthermore, it should be noted that children with diarrhea often have associated comorbidities, such as malnutrition and viral or bacterial infections. These comorbidities may require treatments in addition to ORT, which was not assessed in the Munos et al. study.34 35 36 Organizations including WHO, UNICEF and GiveWell cite the 93% figure, but also note its limitations.37
World Health Organization, and Unicef. “Ending preventable child deaths from pneumonia and Diarrhea by 2025: the integrated global action plan for pneumonia and Diarrhea (GAPPD).” (2013).
Another notable study published in The Lancet in 2003 estimated the potential of ORT and other treatments to prevent all-cause child mortality.38 This study concluded that, in the year 2000, 88% of deaths from diarrheal diseases could have been prevented if available treatments and interventions were used to their full extent. Full coverage of ORT, specifically, could have saved the lives of around 68% of children who died from diarrhea in that year.
More studies are clearly needed. But even if we are cautious and consider these figures overestimates, the evidence still suggests that ORT could be saving hundreds of thousands of more lives if its coverage was increased.
It is worth noting that the potential of ORT does not stop at saving the lives of children. ORT can be used to effectively treat adults as well.39 People aged 70 and older are the largest demographic dying from diarrheal diseases. With increasing numbers of people reaching older age today, the number of older people suffering from diarrhoeal diseases can be expected to grow.
The fact that we are not using ORT to its full potential becomes clear when we look at the distribution of deaths from diarrheal disease among children in different regions: the vast majority of cases occur in South Asia and Sub-Saharan Africa where, as the map above shows, ORT coverage is very low at just 37 and 39 percent, respectively.40
What is so amazing about ORT is not only that it is simple, practical and effective, but, like so many scientific discoveries, once it has been discovered, everyone can benefit from this knowledge. It is what economists call a nonrival good. In fact, Paul Romer, the winner of the 2018 Nobel Memorial Prize in Economic Sciences, often uses ORT as his favourite example of a nonrival good – an idea which does not diminish in its value the more people adopt it and use it.41
Ideas that save millions are far and few between, and ORT is perhaps one of the simplest. We can use simple ideas to solve complex problems, such as how to save the lives of as many children as possible.
Diarrhea is dangerous and life-threatening because it can lead to severe dehydration and electrolyte loss. While drinking water can compensate for some water loss, passive absorption of water through the gut cells is not enough to fully compensate in severe diarrheal cases and the accompanying loss of electrolytes in the stool has negative effects on many bodily functions.
ORT works because of the molecular mechanisms that govern sugar and sodium absorption inside the gut. The cells that make up the lining of the gut have special receptors on their surfaces that allow them to actively absorb sugar molecules. Research by Robert K. Crane and others has shown that the presence of sodium ions in the gut lumen is essential for this process.42 43 44 45
The increase in sugar and sodium inside the cells leads to increased absorption of water and chloride ions as well. When a patient receives a mixture of sugar and salts dissolved in water it offsets the loss of these essential ions and molecules in patients with diarrhea.
The recommended formulation of the amounts of electrolytes and sugars in ORT has changed over time. It’s now often supplemented with other recommended fluids and zinc, which have been shown to improve recovery time and decrease the likelihood of another diarrheal episode in the short term.46
Oral rehydration therapy vs. intravenous rehydration therapy
Despite being a low-tech solution, ORT is highly effective. Recent studies have found no differences between the effectiveness of IVT versus ORT treatments.48
Given that IVT is more invasive and usually requires trained staff, it’s now recommended that ORT is used as a first response measure, switching to IVT only if ORT proves to be ineffective.
In addition, ORT is a much cheaper treatment compared to IVT. According to UNICEF, it costs around $0.50 to provide a course of ORT in lower-income countries and while the saline solution used for IVT is not much more expensive, the additional costs of medical staff, equipment, hospital stay and a longer course of treatment amount to a significant difference in the price of treatment.49
In clinical settings in the UK, ORT has been estimated to be between £351.84 and £630.48 cheaper per course of treatment than IVT.50
ORS composition recommended by the WHO and UNICEF47
While rotavirus is the leading cause of diarrhea in children and therefore, rotavirus vaccine can save the lives of many children, it is not the only cause of diarrhea. To prevent deaths from other diarrheal diarrheal pathogens we need additional interventions and treatments.
Deaths from other diarrheal pathogens, such as cholera or shigella, could be avoided by antibiotics or vaccines, where they are available. But preventions that limit the risks of exposure to diarrheal pathogens in the first place are the key to saving the most lives. Unsafe water and unsafe sanitation contributed to 72% and 56% of the under-5 deaths from diarrheal diseases in 2016. Children who are undernourished, are less likely to survive a diarrheal episode. Consequently, childhood wasting (having a weight too low for their height) is the leading risk factor for diarrheal mortality in children, contributing to an estimated 80% of under-5 deaths from diarrheal diseases in 2016.51
Clearly, eliminating risk factors associated with diarrheal diseases should be on our priority list.